Health Payers
Stay on Track with CMS-0057-F Requirements and Compliance
Are You Ready for Key 2026 Milestones and the 2027 Interoperability Deadline?
The CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) represents one of the most comprehensive shifts in payer operations in recent years — standardizing data exchange, accelerating prior authorization decisions, and increasing transparency across the healthcare ecosystem.
As of January 1, 2026, health plans are required to implement critical operational provisions, including:
-
Accelerated prior authorization decision timelines — standard requests must be completed within 7 calendar days, and expedited requests within 72 hours.
-
Enhanced transparency and reporting, with public disclosure of key prior authorization metrics such as approvals, denials, and turnaround times.
-
Early implementation of electronic prior authorization (ePA) and process transformation across utilization management workflows.
At the same time, the rule’s FHIR-based API requirements — including patient access, provider access, payer-to-payer data exchange, and prior authorization support APIs — are currently targeted for compliance by January 1, 2027, with work in progress throughout 2026 to design, build, and test these capabilities.
Failing to prepare for these milestones can result in operational bottlenecks, inefficiencies, and regulatory risk. From strategic planning to hands-on execution, proactive action this year is essential.
Why Act Now?
2026 is not a “grace period” — it’s a strategic turning point. Even as payers ramp up for full API interoperability in 2027, there are immediate operational requirements and reporting obligations effective now:
-
Achieve consistent turnaround times for prior authorization across all lines of business
-
Support transparent, specific denial explanations for providers and members
-
Publish compliance-ready metrics that withstand CMS scrutiny
With these provisions already in effect, now is the time to operationalize workflows, shore up data capabilities, and embed automation into utilization management.
How Vital Data Technology Helps Health Plans Meet CMS-0057-F Requirements
Vital Data Technology is empowering healthcare payers to meet CMS-0057-F requirements — today and into 2027 — with solutions that unify data, automation, and intelligence across utilization management and interoperability.
Affinitē Intelligent Prior Authorization (IPA)
Our end-to-end CMA-ready prior authorization solution automates and accelerates manual tasks, supports CMS-mandated decision timelines, and ensures accurate, transparent outcomes across standard and expedited reviews.
Affinitē Utilization Management (UM) with CareFlow™ Rules Engine
Design and enforce customizable authorization rules that align with your business and regulatory needs. Built-in workflow automation reduces administrative overhead while improving consistency and compliance.
Advanced Analytics and Reporting
Track and publish prior authorization performance metrics with real-time dashboards and automated reporting pipelines — helping you demonstrate compliance and performance to CMS, providers, and members.
Data Integration and Interoperability Support
Prepare your organization for 2027 API enforcement with support for FHIR standards, data normalization, and integration with provider systems and portals. Whether through expanded Patient Access APIs, Payer-to-Payer exchange, or future ePA integration, VDT has you covered.
Affinitē UM supports CMS-0057-F requirements, including:
-
Advanced analytics and reporting capabilities, including real-time and self-service reporting options.
-
Prior authorization metrics and provider notice, including denial reasons.
-
Support for Medicare Advantage, Medicaid, and Exchange timeliness measures.
-
Advanced data integration and transformation capabilities, including real-time data feeds.
-
Integration with Availity and existing member portals via single sign-on (SSO).
-
Synchronization of benefit coverage and API population with lists of covered items and services requiring prior authorization.
-
Customization of coverage requirements based on specific patient and provider details.
-
Patient Identity Management or Enterprise Master Patient Index (EMPI) capabilities.
-
Support for HL7 FHIR® Da Vinci Coverage Requirements Discovery Implementation Guide, STU 2.0.1.
-
Experience with HL7 FHIR standards, including Patient Access API, Payer-to-Payer API, and Provider Directory API.
-
Conformance with HL7 Clinical Quality Language (CQL) version 1.5.2.
-
Support for Provider Directory API FHIR API system requirements.
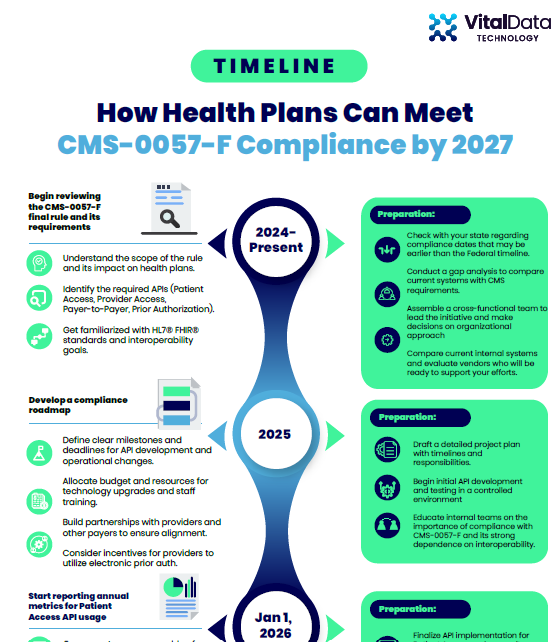
Download the full timeline for a detailed action plan to so you don't miss any important deadlines on the path to implementation!
Timeline: How Health Plans Can Meet CMS-0057-F Compliance by Jan. 1, 2027
Blog
Navigating the 2027 Interoperability and Prior Authorization Rule: Strategies to Consider for Healthcare Payers
The introduction of the 2027 Interoperability and Prior Authorization Rule (CMS-0057-F) by the Centers for Medicare & Medicaid Services (CMS) heralds a pivotal shift in how healthcare payers must operate across the U.S.
This transformative policy is set to redefine data sharing and streamline prior authorization processes, with a clear mandate to enhance patient care and alleviate administrative burdens.
For healthcare payers, this rule presents both a significant challenge and a sizable opportunity to innovate and optimize their operational frameworks.
Your Path to Compliance Starts Here
Whether you are just beginning your compliance journey or refining an existing strategy, VDT’s solutions meet you where you are — helping you build:
-
Operational readiness in 2026 (process, reporting, decision timelines)
-
Technical interoperability foundations for 2027 and beyond
-
Provider and member experiences that support seamless care delivery
Act now to stay ahead of CMS deadlines, reduce administrative costs, and unlock the strategic value of compliant, automated workflows.
Get in touch to discuss how VDT can support your CMS-0057-F compliance journey.

